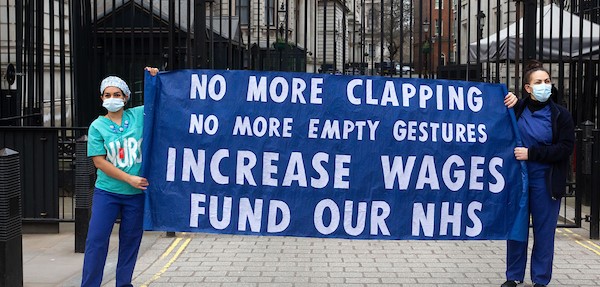
â€Desperate’ NHS funding plea
There’s no doubt that the NHS is under pressure as it faces rising demand and chronic government underfunding.
But seemingly every week new figures reveal just how massive the scale of the crisis facing the health service actually is.
Today (April 7) a new report found that the cases of ambulances being turned away from hospitals have nearly doubled over the last three years.
The Nuffield Trust highlighted figures showing that over this winter, hospitals closed their doors and redirected ambulances to other hospitals a record 478 times.
This was compared to the same time period – between December and February – three years ago, when ambulances were diverted only 249 times.
“There’s rightly been a lot of focus recently on the delays ambulance crews face in being able to hand over their most seriously ill patients at A&E,” said Professor John Appleby, Nuffield Trust chief economist and lead author of the report.
“But what our research today has uncovered is the huge increase in the number of times this winter [that] ambulance trusts have been told they must take patients to another hospital altogether, because an A&E unit simply doesn’t have the capacity to accept any more patients.”
Richard Webber, a practising senior paramedic and national spokesperson for the College of Paramedics explained just why these â€diverts’ as they’re called are so problematic.
â€Double whammy’
“There is a â€double whammy’ in that not only do crews have to drive further away once a divert is implemented – once that’s happened, an ambulance crew will then need to travel further to get back to their own area to respond to the next emergency,” he said.
The skyrocketing number of ambulances being turned away from hospitals comes against a backdrop in which key response time targets have been missed.
Of the more than 200,000 calls made in January classified as Category A – which are the most serious and include cardiac arrest patients – only 88 per cent were met within the response time of 19 minutes, while the target is 95 per cent.
Chair of Unite’s ambulance national organising committee, Debbie Wilkinson, who is also a paramedic in Leeds, explained that there are a number of issues that are stopping the ambulance service from functioning as it should and straining already stretched staff.
“As well as queues and bed blocking, we’re getting calls to a lot of failed discharges (where a patient is sent home too early),” she explained. “Then there’s the amount of inappropriate 111 non-emergency calls that we get directed to.
“I’ve also been sat waiting for two hours for an out-of-hours GP to get back to me, when the minimum reply time is supposed to be half an hour,” said Wilkinson, who works for the Yorkshire Ambulance Service.
“There are constant issues and it’s getting worse,” she added. “The problem is that ambulances rely on hospital and social care services working properly. When they don’t the buck stops with us.”
The Nuffield Trust also found that paramedics suffer from extremely low morale – more so than other NHS staff — as demand increases each year but staffing levels do not keep up.
This dovetails with Unite’s own survey of 362 ambulance staff which the union conducted last year.
Morale
Nearly 90 per cent said morale and motivation at work was falling, with 88 per cent giving the main reason as stress. Ninety-one per cent reported a major increase in workload and 85 per cent said they were working over their contracted hours.
The Nuffield Trust noted that a major concern for ambulance workers was staffing levels – in a separate survey when asked whether there were enough staff to do their jobs properly, 61 per cent disagreed.
Wilkinson echoed the findings reflected in the surveys.
“We’re under tremendous amounts of pressure – the activity rate is going up six per cent annually at the moment but there’s no extra staff, and no extra pay. We’ve had an either 0 or 1 per cent pay rise for the last five years which amounts to a massive pay cut. It’s been hard – really hard.”
As UNITElive reported earlier this year, ambulance cover in the Scottish Highlands has been particularly under strain as it faces a recruitment and management problems.
The crisis there was most recently exemplified in an incident on Wednesday (April 5), when firefighters had to treat a woman hit by a bus in Elgin as they waited 15 minutes for an ambulance to arrive because local ambulance crew were busy attending other emergencies.
Unite regional officer Tommy Campbell said that the incident “goes to show how quickly ambulance cover in Moray can evaporate if several calls come in at once.
“The incident took place very near the fire station, and it is fortunate that firefighters were able to respond so effectively.
“However, this highlights the recurring problem in Moray that overburdened ambulance crews aren’t able to reach casualties as quickly as they should,” he added.
“That boils down to a shortage of vehicles and fully trained staff, which is something the chief executive and her senior management team at the Scottish Ambulance Service must address immediately.”
Labour’s shadow health secretary Jonathan Ashworth said that the government was to blame for the strain the ambulance service and the wider NHS is now under.
“Theresa May has overseen a shocking and unacceptable decline in standards for the NHS this winter,” he said. “Our ambulance services are under increasing pressure and we know that ambulance staff across England are really feeling the strain. They deserve much more support from the government.
“The truth is that years of under-investment by the Conservatives have left hospitals unable to cope with rising demand, and now shocking numbers of ambulances are being diverted because A&Es are stretched to the limits.”
Wilkinson agreed.
“The government must put more funding into the NHS,” she said. “We need it desperately.”
 Like
Like Follow
Follow