‘Fighting a losing battle’
A&E wait times have reached the worst levels since records began, according to the latest NHS figures published this week (February 14).
Hospital A&E units in England have seen only 76.1 per cent of patients within four hours in January, the lowest percentage since the NHS began recording wait times against the target in 2003. A&E units are meant to attend to 95 per cent of patients within four hours.
Hospitals’ failure to cope amid rising pressures has translated into more than 300,000 people having had to endure waits of more than four hours. Another 80,000 people had to undergo so-called â€trolley waits’, where patients wait for four or more hours to be transferred to a ward after their wait in A&E.
Only two major emergency departments in England met the four hour target, while attendances skyrocketed by 85,000 in January compared to the same month last year – another record.
Responding to the latest figures, Nuffield Trust chief economist professor John Appleby said that the figures show that the NHS is “fighting a losing battle in trying to meet its commitments to provide timely health care in the face of the pressure it is under.
“There is a risk that we lose sight of these problems as Brexit distracts us, or become numbed as we forget the last time targets were met,” he added. “But this situation has a serious impact on hundreds of thousands of patients, and will be demoralising for many staff.”
In December, Unite saw the future that today’s January figures confirm, when it said ahead of Christmas that the NHS was facing â€a perfect storm’ winter crisis as ministers energies were diverted by Brexit.
Unite outlined at the time a series of factors contributing to what the union predicted would be among the worst winters for the NHS on record.
Among these factors was a below average annual budget increase; a dramatic 24 per cent decline in the number of health visitors since 2015; another 12 drop in the number of mental health nurses over the last eight years; and a massive number of vacancies throughout the NHS. These vacancies are in jobs as varied as ambulance and paramedic workers; clinical psychologists; mental health nurses; and learning disability support assistants, among others.
Recruitment and retention remains a serious problem in the health service, Unite has found, while the lack of progress in integrating health and social care at a time when the elderly population continues to grow places yet more strain on an NHS that’s already struggling to cope.
Commenting on the latest figures, Unite national officer for health Colenzo Jarrett-Thorpe said that exactly what Unite had predicted in December had come to pass.
“These latest figures show precisely what we at Unite have been saying for some time,” he said. “The worst wait times on record don’t just happen in a vacuum – they’re the result of a combination of government failures, from chronic underfunding the NHS to failing to take action amid an alarming recruitment and retention crisis. We cannot allow Brexit to distract us from an NHS that is well and truly at breaking point, or else waiting times will only become unsustainably worse”.
He explained that the ÂŁ20bn a year injection of extra cash for the NHS by 2023-23 announced by the government last summer is only three per cent a year when historically, since the NHS was founded in 1948, the average has been four per cent.
“The shortfall in funding is glaring,” Jarrett-Thorpe warned.
‘GPs are also struggling
Doctors in Unite (DiU) chair Jackie Applebee agreed.
“At present there is no slack in the system so that when there are high levels of patient activity, especially during winter, waiting times just get longer,” she said.
Like Jarrett-Thorpe, Applebee said that inadequate funding is simply not enough “to keep pace with inflation, a growing population and advances in technology.”
She highlighted that the strain isn’t just hitting hospitals.
“GPs are also struggling,” Applebee said. “Patients often cannot get an appointment for three weeks — a demoralised workforce and chronic underfunding also drive this. The pressure on GPs doesn’t hit the headlines in the same way as we cannot close or declare a black alert when we have too many patients in our waiting rooms; we just get on and see them, often going home very late. No wonder health professionals are burning out.”
Applebee went on to note that the entire NHS workforce is at the end of its tether, working as hard as they possibly can.
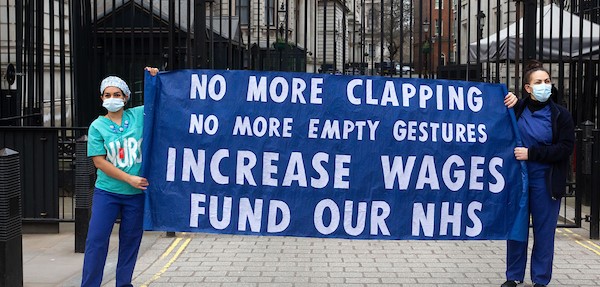
“The NHS is one of the most cost effective health care systems in the developed world, and a recent report showed that NHS productivity was the best in the UK,” she noted. “There is nothing more that health workers can do. Government ministers often laud the NHS — they need to put their money where their mouths are and fund it adequately.”
Jarrett-Thorpe called on the health secretary Matt Hancock and his ministerial team to “refocus their energies on tackling the crisis engulfing the beleaguered NHS, rather than simply, once again, kicking the can down the road, which seems to be the maxim for this government.”
Shadow health secretary Jon Ashworth agreed, calling the latest figures a “damning indictment of years of austerity and wider cuts imposed upon health and care services under the Tories.
“Ministerial incompetence has left our NHS with chronic shortages of NHS staff with no clear idea of how to sort this out,” he added.
“Instead of putting patients first with a clear plan to restore the A&E standard, ministers are looking at scrapping it altogether in the teeth of opposition from the doctors who actually work in A&E departments.”
 Like
Like Follow
Follow